Connect With Us
Blog

Understanding Contagion Risks of Toenail Fungus

Toenail fungus, also known as onychomycosis, is a common fungal infection that affects the nails. This condition is typically characterized by discoloration, thickening, and crumbling of the nails. While toenail fungus is not considered extremely contagious, it can spread from person to person under certain circumstances. Direct contact with infected nails or contaminated surfaces such as shower floors, swimming pools, and communal areas can facilitate transmission. Additionally, sharing shoes, socks, or nail clippers with an infected individual increases the risk of contracting the fungus. Individuals with compromised immune systems, diabetes, or poor circulation are more susceptible to toenail fungus and may experience more severe infections. Maintaining good foot hygiene, wearing breathable footwear, avoiding sharing personal items, and keeping nails trimmed and dry can help reduce the risk of toenail fungus transmission. If you have toenail fungus, it is strongly suggested that you consult a podiatrist who can offer effective treatment remedies, in addition to discussing contamination risks.
If left untreated, toenail fungus may spread to other toenails, skin, or even fingernails. If you suspect you have toenail fungus it is important to seek treatment right away. For more information about treatment, contact Edward Orman, DPM of Honeygo Podiatry. Our doctor can provide the care you need to keep you pain-free and on your feet.
Symptoms
- Warped or oddly shaped nails
- Yellowish nails
- Loose/separated nail
- Buildup of bits and pieces of nail fragments under the nail
- Brittle, broken, thickened nail
Treatment
If self-care strategies and over-the-counter medications does not help your fungus, your podiatrist may give you a prescription drug instead. Even if you find relief from your toenail fungus symptoms, you may experience a repeat infection in the future.
Prevention
In order to prevent getting toenail fungus in the future, you should always make sure to wash your feet with soap and water. After washing, it is important to dry your feet thoroughly especially in between the toes. When trimming your toenails, be sure to trim straight across instead of in a rounded shape. It is crucial not to cover up discolored nails with nail polish because that will prevent your nail from being able to “breathe”.
In some cases, surgical procedure may be needed to remove the toenail fungus. Consult with your podiatrist about the best treatment options for your case of toenail fungus.
If you have any questions, please feel free to contact our offices located in Perry Hall, and Fallston, MD . We offer the newest diagnostic and treatment technologies for all your foot care needs.
How to Treat Your Toenail Fungus
While not a serious issue, toenail fungus, or onychomycosis, can be an embarrassing and uncomfortable condition to experience. Toenail fungus is often caused from public areas that harbor fungi and improper cleaning/drying of the foot. Once infected, the fungus grows deeper into the nail and can be very hard to get rid of.
There are different types of fungus that cause toenail fungus. Dermatophytes, yeasts, and molds are the most frequent forms of fungus to infect the toenail. Dermatophytes are the most common among the three. Symptoms associated with fungal nails include the discoloration of the toenail, brittleness, and in some circumstances, a smell. Pain is rarely a symptom caused by toenail fungus.
Diagnosis of fungal nails is generally a rather quick process. However podiatrists will make sure that the cause is not another condition such as lichen planus, psoriasis, onychogryphosis, or nail damage. Podiatrists will make use of fungal cultures and microscopy to verify that it is fungus.
While over-the-counter ointments are readily available, most are ineffective. This is due to the fact that the nail is very protective and that the fungus slips in between the nail plate and bed. Podiatrists can offer oral medication which currently provides the best results.
Ultimately, prevention is the best line of defense against toenail fungus. Avoid unsanitary public showers. If you do use a public shower, use shower shoes to provide your foot with protection. Once you are finished showering, make sure to thoroughly dry your feet. Fungi thrive in warm, dark, and moist places like sweaty, warm feet that are left dark in shoes all day.
The Essence of Podiatry

Podiatry, a branch of medicine dedicated to the study, diagnosis, and treatment of disorders related to the foot, ankle, and lower extremities, plays a pivotal role in maintaining overall health and mobility. Podiatrists, also known as foot doctors, undergo extensive training to specialize in the intricate structure and function of the feet and ankles. Their expertise encompasses a wide range of conditions, including bunions, plantar fasciitis, ingrown toenails, heel spurs, and diabetic foot complications. Podiatrists employ various diagnostic techniques such as physical examinations, imaging studies, and biomechanical assessments to evaluate foot problems accurately. Treatment modalities may include conservative measures like orthotics, custom footwear, and medication, as well as surgical interventions for more severe conditions. Additionally, podiatrists play a vital role in preventive care, educating patients about proper foot hygiene, footwear choices, and injury prevention strategies. By addressing foot-related issues comprehensively, podiatrists help enhance the quality of life, promote mobility, and prevent debilitating complications associated with foot disorders. If you have foot or ankle discomfort or are interested in learning more about the field of podiatry, it is suggested that you speak to this type of doctor who can provide you with the care and the knowledge you are seeking.
If you are experiencing pain in the feet or ankles, don’t join the stubborn majority refusing treatment. Feel free to contact Edward Orman, DPM from Honeygo Podiatry. Our doctor can provide the care you need to keep you pain-free and on your feet.
What Is a Podiatrist?
Someone would seek the care of a podiatrist if they have suffered a foot injury or have common foot ailments such as heal spurs, bunions, arch problems, deformities, ingrown toenails, corns, foot and ankle problems, etc.
Podiatric Treatment
A podiatrist will treat the problematic areas of the feet, ankle or lower leg by prescribing the following:
- Physical therapy
- Drugs
- Orthotic inserts or soles
- Surgery on lower extremity fractures
A common podiatric procedure a podiatrist will use is a scanner or force plate which will allow the podiatrist to know the designs of orthotics. Patients are then told to follow a series of tasks to complete the treatment. The computer will scan the foot a see which areas show weight distribution and pressure points. The podiatrist will read the analysis and then determine which treatment plans are available.
If you have any questions please feel free to contact our offices located in Perry Hall, and Fallston, MD . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
What is a Podiatrist?
A podiatrist is a Doctor of Podiatric Medicine who treats the foot, ankle, and related structures of the leg. If you are having any pain, injuries, or abnormalities in these areas, it is best that you seek help from a podiatrist.
Podiatrists complete four years of training in a podiatric medical school. Their training is like that of other physicians, and they may go on to complete a fellowship training after a residency training. Some podiatrists are board certified meaning they have advanced training, clinical experience, and have taken an exam to prove their skills. Certifying boards for podiatry are the American Board of Foot and Ankle Surgery and the American Board of Podiatric Medicine. Podiatrists may work in private practices, hospitals, clinics, or they may even become professors at colleges of podiatric medicine.
While in college, those who want to be podiatrists often take biology, chemistry, and physics classes in preparation for podiatry school. In podiatry school, students study how the bones, nerves, and muscles work together to help you move around. Additionally, they study injuries and how to properly diagnose and treat them. Admittance into podiatric medical school requires the completion of 90 semester hours of undergraduate study with a good grade point average, and acceptable scores on the MCAT (Medical College Admission Test)
Podiatrists treat many different conditions such as: aching feet, ankle pain, bunions, corns, hammertoes, fungus, ingrown toenails, plantar fasciitis, sprains and more. Common forms of treatment for these conditions are physical therapy, drugs, or surgery. Podiatrists may also recommend corrective shoe inserts, custom-made shoes, plaster casts, and strappings to correct deformities.
Even if you are someone whose feet are in generally good condition, you should still visit a podiatrist to have your feet properly exfoliated and maintained, or to make sure you are looking after your feet properly.
Risk Factors for Sprained Ankles

Understanding the risk factors for ankle sprains and strains is important to avoid injury. Poor athletic conditioning, characterized by a lack of regular ankle strengthening exercises, increases susceptibility to ankle sprains during strenuous activities. Muscle and ligament fatigue, especially when pushing through exhaustion towards the end of vigorous activities, further heightens the risk. Skipping warm-up sessions before physical activity leaves muscles and ligaments tight, while decreasing flexibility and increasing vulnerability to injury. Excess weight places additional stress on the joints, amplifying the likelihood of sprains during movements like walking, running, or jumping. Gender and age also play significant roles, with females over 30 and males aged 15 to 24 showing higher susceptibility to ankle sprains. Wearing high heels in uneven terrain, and wearing low-topped shoes during sports like basketball, further increases the risk of injury. Through proper conditioning, warm-up routines, weight management, and appropriate footwear selection, the risk of ankle sprains decreases. For personalized guidance and strategies for minimizing ankle sprain risk, it is suggested that you schedule an appointment with a podiatrist.
Although ankle sprains are common, they aren’t always minor injuries. If you need your ankle injury looked at, contact Edward Orman, DPM from Honeygo Podiatry. Our doctor can provide the care you need to keep you pain-free and on your feet.
How Does an Ankle Sprain Occur?
Ankle sprains are the result of a tear in the ligaments within the ankle. These injuries may happen when you make a rapid shifting movement while your foot is planted. A less common way to sprain your ankle is when your ankle rolls inward while your foot turns outward.
What Are the Symptoms?
- Pain at the sight of the tear
- Bruising/Swelling
- Ankle area is tender to touch
- In severe cases, may hear/feel something tear
- Skin discoloration
Preventing a Sprain
- Wearing appropriate shoes for the occasion
- Stretching before exercises and sports
- Knowing your limits
Treatment of a Sprain
In many cases, the RICE method (Rest, Ice, Compression, and Elevate) is used to treat ankle sprains. However, you should see a podiatrist to see which treatment option would work best with your injury. In severe cases, surgery may be required.
It is important to ask your doctor about rehab options after you receive treatment for your injury. Stretching, strength training, and balance exercises may help the ankle heal while also preventing further injury.
If you have any questions, please feel free to contact our offices located in Perry Hall, and Fallston, MD . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Ankle Sprains
Ankle sprains occur when ligaments that support the ankle stretch beyond their limits and tear. These types of injuries are very common and can occur in people of all ages. Sprains may range from mild to severe, depending on how much damage is done to the ligaments. If a sprain goes untreated, a more severe sprain may occur which can further damage the ankle. Repeated ankle sprains can lead to chronic ankle pain.
There are some risk factors that can increase your risk of suffering a sprained ankle. Those who participate in sports, walk on uneven surfaces, have a prior ankle injury, are in poor physical condition, or wear improper shoes are more likely to get a sprained ankle.
There are a few symptoms to look out for if you suspect you are suffering from a sprained ankle. Some common symptoms are swelling, bruising, tenderness, and instability of the ankle. In cases where the tearing of the ligaments is severe, there may be a “popping” sound when the strain occurs.
The RICE method is proven to be effective in treating ankle sprains. RICE stands for Rest, Ice, Compression, and Elevation. Rest is important for treatment, especially within the first 24 to 48 hours. You should also ice your sprained ankle for the first 48 hours for 20 minutes at a time. A small piece of cloth should be placed between the ice and the affected area. For the compression step, you should wear a brace that is snug, but not too tight that it cuts off circulation. When choosing a brace, be sure to choose one that is suitable for the type of ankle sprain you have. Lastly, you should elevate your foot above the heart as often as possible.
After you treat a sprain, you should go through rehabilitation to prevent the injury from occurring again. There are three phases to the rehab process. The first phase involves resting, protecting, and reducing the swelling of the injury. The second phase consists of restoring the ankle’s flexibility, range of motion, and strength. The third phase consists of slowly returning to activity and maintenance exercises.
If you suspect you have an ankle sprain, you shouldn’t hesitate to consult with your podiatrist. Your podiatrist will be able to give you a proper diagnosis and a suitable treatment option for your condition.
Arthritis Can Cause Pain in the Feet and Ankles
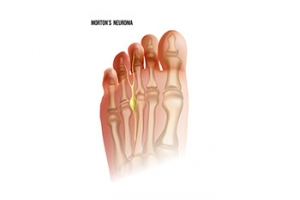
Common Symptoms of Morton’s Neuroma
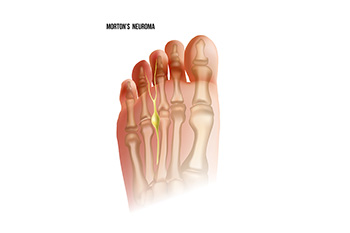
Morton's neuroma is a painful condition that affects the ball of the foot, specifically the area between the third and fourth toes. This condition involves the thickening of the tissue surrounding a nerve leading to the toes, usually caused by irritation or compression. The hallmark symptom of Morton's neuroma is a sharp, burning pain or the sensation of a small, pebble-like object under the ball of the foot. As the condition progresses, individuals may experience numbness, tingling, or a feeling of swelling in the toes. The pain tends to worsen with activities like walking or wearing tight shoes, as these activities compress the affected nerve. Morton's neuroma is often more prevalent in women and individuals who frequently wear high heels or engage in activities that put repetitive pressure on the forefoot. Morton’s neuroma is treated by a podiatrist. If you are experiencing symptoms of this condition, it is suggested that you schedule an appointment with this type of doctor who can accurately diagnose and treat Morton’s neuroma.
Morton’s neuroma is a very uncomfortable condition to live with. If you think you have Morton’s neuroma, contact Edward Orman, DPM of Honeygo Podiatry. Our doctor will attend to all of your foot care needs and answer any of your related questions.
Morton’s Neuroma
Morton's neuroma is a painful foot condition that commonly affects the areas between the second and third or third and fourth toe, although other areas of the foot are also susceptible. Morton’s neuroma is caused by an inflamed nerve in the foot that is being squeezed and aggravated by surrounding bones.
What Increases the Chances of Having Morton’s Neuroma?
- Ill-fitting high heels or shoes that add pressure to the toe or foot
- Jogging, running or any sport that involves constant impact to the foot
- Flat feet, bunions, and any other foot deformities
Morton’s neuroma is a very treatable condition. Orthotics and shoe inserts can often be used to alleviate the pain on the forefront of the feet. In more severe cases, corticosteroids can also be prescribed. In order to figure out the best treatment for your neuroma, it’s recommended to seek the care of a podiatrist who can diagnose your condition and provide different treatment options.
If you have any questions, please feel free to contact our offices located in Perry Hall, and Fallston, MD . We offer the newest diagnostic and treatment technologies for all your foot care needs.
What is Morton's Neuroma?
Morton’s neuroma, (also referred to as Morton’s metatarsalgia, Morton’s neuralgia, plantar neuroma or intermetatarsal neuroma) is a condition that is caused when the tissue around one of the nerves between your toes begins to thicken. This thickening can result in pain in the ball of the foot. Fortunately, the condition itself is not cancerous.
Morton’s neuroma affects women more often than men with a ratio of 4:1. It tends to target women between the age of 50 and 60, but it can occur in people of all ages. There are some risk factors that may put you at a slightly higher risk of developing the condition. People who often wear narrow or high-heeled shoes are often found to be linked to Morton’s neuroma. Additionally, activities such as running or jogging can put an enormous amount of pressure on the ligament and cause the nerve to thicken.
There usually aren’t any outward symptoms of this condition. A person who has Morton’s neuroma may feel as if they are standing on a pebble in their shoe. They may also feel a tingling or numbness in the toes as well as a burning pain in the ball of their foot that may radiate to their toes.
In order to properly diagnose you, the doctor will press on your foot to feel for a mass or tender spot. He may also do a series of tests such as x-rays, an ultrasound, or an MRI. X-rays are usually done to rule out any other causes for your foot pain such as a stress fracture. Ultrasounds are used to reveal soft tissue abnormalities that may exist, such as neuromas. Your podiatrist may want to use an MRI in order to visualize your soft tissues.
There are three main options for treatment of Morton’s neuroma: Injections, decompression surgery, and removal of the nerve. Injections of steroids into the painful area have been proven to help those with Morton’s neuroma. Decompression surgery has been shown to relieve pressure on the affected nerve by cutting nearby structures such as the ligaments in the foot. Another treatment option would be to surgically remove the growth to provide pain relief.
If you suspect that you have Morton’s neuroma you should make an appointment with your podiatrist right away. You shouldn’t ignore any foot pain that lasts longer than a few days, especially if the pain does not improve.
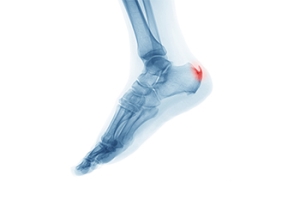
Definition and Symptoms of Heel Spurs
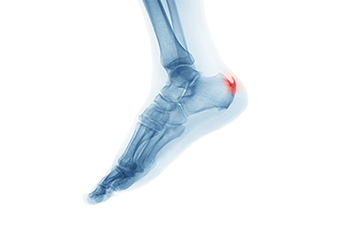
Heel spurs are bony protrusions that develop on the underside of the heel bone, often causing discomfort and pain. These spurs typically form in response to long-term strain on the ligaments and muscles of the foot, which leads to the calcification of soft tissues near the heel. While some individuals with heel spurs may not experience any symptoms, others may encounter persistent pain, especially during weight-bearing activities such as walking or standing. The pain is often described as a sharp, stabbing sensation in the heel. Inflammation and tenderness may accompany the discomfort, further affecting mobility. Seeking professional evaluation from a podiatrist is essential for an accurate diagnosis and the formulation of an effective treatment plan to alleviate symptoms and enhance overall foot health. If you have a heel spur, it is suggested that you consult with this type of doctor who can accurately diagnose and treat this condition.
Heel spurs can be incredibly painful and sometimes may make you unable to participate in physical activities. To get medical care for your heel spurs, contact Edward Orman, DPM from Honeygo Podiatry. Our doctor will do everything possible to treat your condition.
Heels Spurs
Heel spurs are formed by calcium deposits on the back of the foot where the heel is. This can also be caused by small fragments of bone breaking off one section of the foot, attaching onto the back of the foot. Heel spurs can also be bone growth on the back of the foot and may grow in the direction of the arch of the foot.
Older individuals usually suffer from heel spurs and pain sometimes intensifies with age. One of the main condition's spurs are related to is plantar fasciitis.
Pain
The pain associated with spurs is often because of weight placed on the feet. When someone is walking, their entire weight is concentrated on the feet. Bone spurs then have the tendency to affect other bones and tissues around the foot. As the pain continues, the feet will become tender and sensitive over time.
Treatments
There are many ways to treat heel spurs. If one is suffering from heel spurs in conjunction with pain, there are several methods for healing. Medication, surgery, and herbal care are some options.
If you have any questions feel free to contact our offices located in Perry Hall, and Fallston, MD . We offer the latest in diagnostic and treatment technology to meet your needs.
Blog Archives
- June 2025
- May 2025
- April 2025
- March 2025
- February 2025
- January 2025
- December 2024
- November 2024
- October 2024
- September 2024
- August 2024
- July 2024
- June 2024
- May 2024
- April 2024
- March 2024
- February 2024
- January 2024
- December 2023
- November 2023
- October 2023
- September 2023
- August 2023
- July 2023
- June 2023
- May 2023
- April 2023
- March 2023
- February 2023
- January 2023
- December 2022