Connect With Us
Blog

Managing Infected Ingrown Toenails

Ingrown toenails, a common problem causing pain and inconvenience, can affect anyone. However, they are most frequently seen in young adults and adolescents. These toenails usually affect the big toe but can affect other toes as well. Causes of ingrown toenails include direct trauma to the toe, genetic predisposition, improper nail trimming, and wearing poorly fitting shoes. There are three stages of ingrown toenails. Stage one involves redness, slight swelling, and pain at the lateral nail fold. Stage two presents with increased pain, discharge from the nail edge, and signs of bacterial paronychia. In stage three, hypertrophic granulation tissue forms on the lateral wall. Treatment ranges from the conservative to surgery. If you have an ingrown toenail, particularly if it appears infected, it is suggested that you schedule an appointment with a podiatrist to have the affected nail evaluated, and proper treatment given.
Ingrown toenails may initially present themselves as a minor discomfort, but they may progress into an infection in the skin without proper treatment. For more information about ingrown toenails, contact Edward Orman, DPM of Honeygo Podiatry. Our doctor can provide the care you need to keep you pain-free and on your feet.
Ingrown Toenails
Ingrown toenails are caused when the corner or side of a toenail grows into the soft flesh surrounding it. They often result in redness, swelling, pain, and in some cases, infection. This condition typically affects the big toe and may recur if it is not treated properly.
Causes
- Improper toenail trimming
- Genetics
- Improper shoe fitting
- Injury from pedicures or nail picking
- Abnormal gait
- Poor hygiene
You are more likely to develop an ingrown toenail if you are obese, have diabetes, arthritis, or have any fungal infection in your nails. Additionally, people who have foot or toe deformities are at a higher risk of developing an ingrown toenail.
Symptoms
Some symptoms of ingrown toenails are redness, swelling, and pain. In rare cases, there may be a yellowish drainage coming from the nail.
Treatment
Ignoring an ingrown toenail can have serious complications. Infections of the nail border can progress to a deeper soft-tissue infection, which can then turn into a bone infection. You should always speak with your podiatrist if you suspect you have an ingrown toenail, especially if you have diabetes or poor circulation.
If you have any questions, please feel free to contact our offices located in Perry Hall, and Fallston, MD . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Ingrown Toenails
Ingrown toenails (onychocryptosis) are a common foot ailment and it is very unpleasant to experience. The condition is caused by an increase in pressure from the ingrowth of the nail edge into the skin of the toe. Ingrown toenails commonly cause pain in those who experience them. In some cases, the skin surrounding the ingrown toenail may break which may lead bacteria to enter through and cause an infection. Common symptoms of this ailment include pain, redness, swelling, and warmth around the toe.
An imbalance between the size of the nail and the enlargement of the nail skin edge causes ingrown toenails. This condition is often caused by improperly trimming the toenails. If you are trying you cut your nails, you should always try to trim straight across instead of in a rounded shape. Ingrown toenails can also be an inherited condition and they may also be caused by improper shoe fitting.
Another common cause of the condition is wearing shoes that are either too small or too large. Other causes include poor foot hygiene, obesity, diabetes, arthritis, edema, and fungal infections. There are many risk factors that may make a person more likely to develop an ingrown toenail. Athletes who play “stop and start” sports such as tennis, soccer, and basketball are most likely to have ingrown toenails.
People who have diabetes, a compromised immune system, or poor circulation should immediately seek care from a podiatrist if they have an ingrown toenail. It is also recommended to seek professional assistance if at-home remedies are not successful within a week or if there is persistent pain.
Are Bunions Affecting Your Everyday Life?
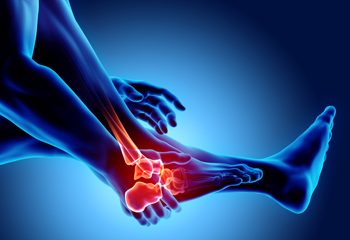
Causes and Definition of Tarsal Tunnel Syndrome

Tarsal tunnel syndrome, a condition affecting the inner ankle and foot, arises from compression of the tibial nerve within the tarsal tunnel. This tunnel, enclosed by bone and soft tissues, houses nerves, arteries, and tendons. When pressure on the tibial nerve increases, it can result in tarsal tunnel syndrome. Causes vary, with one primary factor being overuse, leading to inflammation and swelling within the tunnel. Flat feet or conditions altering foot biomechanics may contribute by narrowing the tunnel and compressing the nerve. Ankle injuries, cysts, or tumors within the tunnel can exacerbate the compression, as can systemic conditions like diabetes or arthritis. Symptoms encompass tingling, burning sensations, and pain radiating to the arch, heel, or toes. Recognizing these indicators and understanding the diverse causes of tarsal tunnel syndrome is vital for timely intervention. If you have foot pain, it is strongly suggested that you schedule an appointment with a podiatrist who can diagnose and treat tarsal tunnel syndrome.
Tarsal tunnel syndrome can be very uncomfortable to live with. If you are experiencing tarsal tunnel syndrome, contact Edward Orman, DPM of Honeygo Podiatry. Our doctor can provide the care you need to keep you pain-free and on your feet.
Tarsal Tunnel Syndrome
Tarsal tunnel syndrome, which can also be called tibial nerve dysfunction, is an uncommon condition of misfiring peripheral nerves in the foot. The tibial nerve is the peripheral nerve in the leg responsible for sensation and movement of the foot and calf muscles. In tarsal tunnel syndrome, the tibial nerve is damaged, causing problems with movement and feeling in the foot of the affected leg.
Common Cause of Tarsal Tunnel Syndrome
- Involves pressure or an injury, direct pressure on the tibial nerve for an extended period of time, sometimes caused by other body structures close by or near the knee.
- Diseases that damage nerves, including diabetes, may cause tarsal tunnel syndrome.
- At times, tarsal tunnel syndrome can appear without an obvious cause in some cases.
The Effects of Tarsal Tunnel Syndrome
- Different sensations, an afflicted person may experience pain, tingling, burning or other unusual sensations in the foot of the affected leg.
- The foot muscles, toes and ankle become weaker, and curling your toes or flexing your foot can become difficult.
- If condition worsens, infections and ulcers may develop on the foot that is experiencing the syndrome.
A physical exam of the leg can help identify the presence of tarsal tunnel syndrome. Medical tests, such as a nerve biopsy, are also used to diagnose the condition. Patients may receive physical therapy and prescriptive medication. In extreme cases, some may require surgery.
If you have any questions please feel free to contact our offices located in Perry Hall, and Fallston, MD . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Tarsal Tunnel Syndrome
Tarsal tunnel syndrome is a condition in which there is a compression of the posterior tibial nerve. The posterior tibial nerve runs along the inside of the ankle into the foot. Tarsal tunnel syndrome is named for the tarsal tunnel, which is a thin space along the inside of the ankle beside the ankle bones. This space contains various nerves, arteries, and tendons, and includes the posterior tibial nerve. The tibial nerve is the peripheral nerve in the leg responsible for sensation and movement of the foot and calf muscles. In tarsal tunnel syndrome the tibial nerve is compressed, causing tingling or burning, numbness, and pain.
Common causes of tarsal tunnel syndrome involve pressure or an injury. Injuries that produce inflammation and swelling in or around the tunnel may place pressure on the posterior tibial nerve. Direct pressure on the tibial nerve for an extended period of time, sometimes caused by other body structures close by or trauma to the tibial nerve, can result in tarsal tunnel syndrome. Diseases that damage nerves, such as diabetes or arthritis, may cause tarsal tunnel syndrome. Those with flat feet are at risk for developing the condition, as the extra pressure and strain placed on the foot may compress the posterior tibial nerve.
Feeling different sensations in the foot at different times is a common symptom of tarsal tunnel syndrome. An afflicted person may experience pain, tingling, burning or other unusual sensations in the foot of the affected leg. Symptoms are primarily felt on bottom of the foot and/or the inside of the ankle. Symptoms can appear suddenly and may occur due to overuse of the foot.
To diagnose tarsal tunnel syndrome, your podiatrist may examine the foot and tap the posterior tibial nerve to see if symptoms surface. He or she may also order an MRI to determine if a mass is present.
Treating tarsal tunnel syndrome will depend on the decision of your podiatrist. Multiple options are available, however, and can include rest, ice, immobilization, oral medications such as anti-inflammatory drugs (NSAIDS), physical therapy, injection therapy, orthotics, supportive shoes, braces, and surgery.
Foot Pain
The feet, being the foundation of the body, carry all of the body’s weight and are therefore prone to experiencing pain and discomfort. If you are experiencing foot pain, it is important to determine where in the foot you are experiencing this pain to help discover the cause of it. While pain can be experienced virtually anywhere in the foot, the most common sites of foot pain are in the heel and ankle.
Heel pain can be due to a multitude of conditions including plantar fasciitis, Achilles tendinitis, and heel spurs. Pain experienced in the ankle can be a sign of an ankle sprain, arthritis, gout, ankle instability, ankle fracture, or nerve compression. In more serious cases, pain in the foot can be a sign of improper alignment or an infection.
Foot pain can be accompanied by symptoms including redness, swelling, stiffness and warmth in the affected area. Whether the pain can be described as sharp or dull depends on the foot condition behind it. It is important to visit your local podiatrist if your foot pain and its accompanying symptoms persist and do not improve over time.
Depending on the location and condition of your foot pain, your podiatrist may prescribe certain treatments. These treatments can include but are not limited to prescription or over-the-counter drugs and medications, certain therapies, cortisone injections, or surgery.
If you are experiencing persistent foot pain, it is important to consult with your foot and ankle doctor to determine the cause and location. He or she will then prescribe the best treatment for you. While milder cases of foot pain may respond well to rest and at-home treatments, more serious cases may take some time to fully recover.
Understanding What Arthritis in the Feet Feels Like
Arthritis in the feet is a condition that can bring a range of discomforts and unique sensations. It often manifests as pain and stiffness in the joints, making every step a potential challenge. Individuals with foot arthritis may experience a deep, aching pain that worsens with movement. This discomfort can be present in various areas of the foot, including the toes, the midfoot, or the ankle. One common sensation associated with foot arthritis is a feeling of stiffness or inflexibility. It can be particularly pronounced in the morning or after periods of inactivity. As arthritis progresses, swelling and warmth may accompany the pain, making the affected foot feel tender to the touch. In more advanced cases, individuals may notice a grinding or popping sensation in the affected joints, indicating the wear and tear of the cartilage. Understanding what arthritis in the feet feels like is essential for timely diagnosis and effective management. If you have any of the above symptoms which may indicate arthritis in the feet, it is suggested that you schedule an appointment with a podiatrist who can guide you toward relief methods.
Arthritis can be a difficult condition to live with. If you are seeking treatment, contact Edward Orman, DPM from Honeygo Podiatry. Our doctor can provide the care you need to keep you pain-free and on your feet.
Arthritic Foot Care
Arthritis is a term that is commonly used to describe joint pain. The condition itself can occur to anyone of any age, race, or gender, and there are over 100 types of it. Nevertheless, arthritis is more commonly found in women compared to men, and it is also more prevalent in those who are overweight. The causes of arthritis vary depending on which type of arthritis you have. Osteoarthritis for example, is often caused by injury, while rheumatoid arthritis is caused by a misdirected immune system.
Symptoms
- Swelling
- Pain
- Stiffness
- Decreased Range of Motion
Arthritic symptoms range in severity, and they may come and go. Some symptoms stay the same for several years but could potentially get worse with time. Severe cases of arthritis can prevent its sufferers from performing daily activities and make walking difficult.
Risk Factors
- Occupation – Occupations requiring repetitive knee movements have been linked to osteoarthritis
- Obesity – Excess weight can contribute to osteoarthritis development
- Infection – Microbial agents can infect the joints and trigger arthritis
- Joint Injuries – Damage to joints may lead to osteoarthritis
- Age – Risk increases with age
- Gender –Most types are more common in women
- Genetics – Arthritis can be hereditary
If you suspect your arthritis is affecting your feet, it is crucial that you see a podiatrist immediately. Your doctor will be able to address your specific case and help you decide which treatment method is best for you.
If you have any questions, please feel free to contact our offices located in Perry Hall, and Fallston, MD . We offer the newest diagnostic and treatment technologies for all your foot care needs.
How to Care for Your Arthritic Foot
Arthritis is an inflammation of the joints and it can occur at any joint in the body, especially in the foot. It generally effects those who are older, however, it can occur at any age. Although there are many different forms of arthritis, there are three main types that occur in the foot. The three types are osteoarthritis, rheumatoid arthritis, and gout.
The primary cause of osteoarthritis is aging. As you age, cartilage degenerates around the joints which causes friction and pain. Obesity can cause osteoarthritis through mechanical stress. Injuries that damage joints can increase the probability as well. Finally, a family history of osteoarthritis can also increase chances of having it.
Rheumatoid arthritis occurs when the immune system attacks the joint linings and weakens them over a long time. While there is no known cause of rheumatoid arthritis, obesity and smoking can increase your chances of getting it. Women are also more likely to get it than men.
Gout is a form of arthritis that occurs when there is too much uric acid in your blood and painful crystals form in your joints. Men are more likely to have gout than women. People who are obese or drink alcohol often are also more likely to develop gout. Furthermore, having diabetes, heart disease, high blood pressure, high cholesterol, gastric bypass surgery or a family history of gout may increase your likelihood of developing the condition.
Symptoms of arthritis include pain, stiffness, swelling in the joints. These symptoms can make it harder and more painful to walk. Physical activity can increase pain and discomfort. Furthermore, joint pain can worsen throughout the day for osteoarthritis. Gout attacks generally last several days with the first few being the worst.
Diagnosis of gout includes either a joint fluid test or a blood test. X-ray imaging can detect osteoarthritis but not gout. On the other hand, there is no blood test for osteoarthritis. Rheumatoid arthritis is difficult to diagnosis. Doctors utilize family and personal medical history, a physical examination, and antibody blood tests to determine if you have rheumatoid arthritis.
Treatment varies for the different kinds of arthritis. Anti-inflammatory medication or steroids can help reduce pain from inflammation of the joints. Changing shoe types can help with some symptoms. Wider shoes can help with discomfort from gout and osteoarthritis. High heels should be avoided. Shoes with proper arch support and that take pressure off the ball of the foot can help with rheumatoid arthritis. Drinking lots of water can also help rid uric acid from the blood. Losing weight, improving your diet, and limiting alcohol and smoking can also help prevent or lessen the symptoms of arthritis.
If you are having trouble walking or pain in your feet, see a podiatrist to check if you have arthritis.
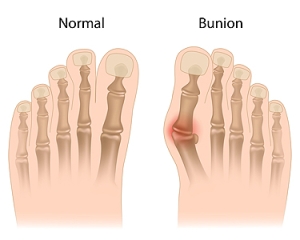
Causes and Treatment for Bunions
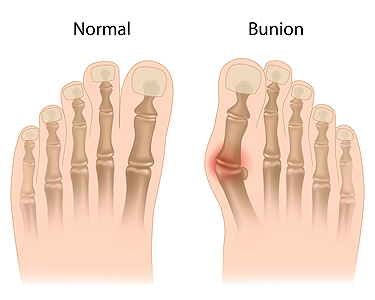
Bunions are painful bumps at the base of the big toe, primarily the result of hallux valgus, where the big toe deviates outward and tilts toward the second toe. Contributing factors for the formation of bunions include foot pronation, wearing tight shoes, injuries, osteoarthritis, and heredity. Bunions can cause pain, especially in narrow shoes, and may enlarge over time. Painful swelling caused by inflamed bursa under the toe often accompanies bunions and limits joint motion. Diagnosing bunions relies on symptoms and physical exams, such as X-rays, while joint fluid analysis rules out infectious arthritis or gout. Treatment options depend on the severity of the bunion. A podiatrist can guide you toward non-invasive treatment solutions, including orthotics, nonsteroidal anti-inflammatory medication, and corticosteroid injections to manage pain and inflammation. In severe cases, or when more conservative measures fail, surgical bunionectomy becomes an option. This procedure corrects joint alignment and removes the bunion. To determine the best treatment plan for your specific needs and taking into account the severity of your bunion, it is suggested that you make an appointment with a podiatrist.
If you are suffering from bunions, contact Edward Orman, DPM of Honeygo Podiatry. Our doctor can provide the care you need to keep you pain-free and on your feet.
What Is a Bunion?
A bunion is formed of swollen tissue or an enlargement of boney growth, usually located at the base joint of the toe that connects to the foot. The swelling occurs due to the bones in the big toe shifting inward, which impacts the other toes of the foot. This causes the area around the base of the big toe to become inflamed and painful.
Why Do Bunions Form?
Genetics – Susceptibility to bunions are often hereditary
Stress on the feet – Poorly fitted and uncomfortable footwear that places stress on feet, such as heels, can worsen existing bunions
How Are Bunions Diagnosed?
Doctors often perform two tests – blood tests and x-rays – when trying to diagnose bunions, especially in the early stages of development. Blood tests help determine if the foot pain is being caused by something else, such as arthritis, while x-rays provide a clear picture of your bone structure to your doctor.
How Are Bunions Treated?
- Refrain from wearing heels or similar shoes that cause discomfort
- Select wider shoes that can provide more comfort and reduce pain
- Anti-inflammatory and pain management drugs
- Orthotics or foot inserts
- Surgery
If you have any questions, please feel free to contact our offices located in Perry Hall, and Fallston, MD . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Bunions
A bunion is an enlargement of the base joint of the toe that connects to the foot, often formed from a bony growth or a patch of swollen tissues. It is caused by the inward shifting of the bones in the big toe, toward the other toes of the foot. This shift can cause a serious amount of pain and discomfort. The area around the big toe can become inflamed, red, and painful.
Bunions are most commonly formed in people who are already genetically predisposed to them or other kinds of bone displacements. Existing bunions can be worsened by wearing improperly fitting shoes. Trying to cram your feet into high heels or running or walking in a way that causes too much stress on the feet can exacerbate bunion development. High heels not only push the big toe inward, but shift one's body weight and center of gravity towards the edge of the feet and toes, expediting bone displacement.
A podiatrist knowledgeable in foot structure and biomechanics will be able to quickly diagnose bunions. Bunions must be distinguished from gout or arthritic conditions, so blood tests may be necessary. The podiatrist may order a radiological exam to provide an image of the bone structure. If the x-ray demonstrates an enlargement of the joint near the base of the toe and a shifting toward the smaller toes, this is indicative of a bunion.
Wearing wider shoes can reduce pressure on the bunion and minimize pain, and high heeled shoes should be eliminated for a period of time. This may be enough to eliminate the pain associated with bunions; however, if pain persists, anti-inflammatory drugs may be prescribed. Severe pain may require an injection of steroids near the bunion. Orthotics for shoes may be prescribed which, by altering the pressure on the foot, can be helpful in reducing pain. These do not correct the problem; but by eliminating the pain, they can provide relief.
For cases that do not respond to these methods of treatment, surgery can be done to reposition the toe. A surgeon may do this by taking out a section of bone or by rearranging the ligaments and tendons in the toe to help keep it properly aligned. It may be necessary even after surgery to wear more comfortable shoes that avoid placing pressure on the toe, as the big toe may move back to its former orientation toward the smaller toes.
Blog Archives
- December 2025
- November 2025
- October 2025
- September 2025
- August 2025
- July 2025
- June 2025
- May 2025
- April 2025
- March 2025
- February 2025
- January 2025
- December 2024
- November 2024
- October 2024
- September 2024
- August 2024
- July 2024
- June 2024
- May 2024
- April 2024
- March 2024
- February 2024
- January 2024
- December 2023
- November 2023
- October 2023
- September 2023
- August 2023
- July 2023
- June 2023
- May 2023
- April 2023
- March 2023
- February 2023
- January 2023