Connect With Us
Blog
Blog
Nerve Problems in Children Are Often Linked to Other Health Conditions

Some children develop nerve issues in the feet and legs as a result of other medical conditions affecting their entire body. These nerve problems, known as peripheral nerve disorders, can cause tingling, numbness, weakness, or burning sensations. In children, they may be connected to illnesses such as diabetes, autoimmune disorders, or infections. When these underlying health conditions affect how nerves send signals, it can lead to trouble with walking, balance, or coordination. Early signs are sometimes subtle, like frequent tripping or unexplained foot discomfort. Identifying the root cause is important, as treating the overall condition often improves nerve symptoms. If a child begins to show signs of nerve changes or foot pain without injury, it is suggested that you visit a podiatrist for further investigation.
Peripheral artery disease can pose a serious risk to your health. It can increase the risk of stroke and heart attack. If you have symptoms of peripheral artery disease, consult with Edward Orman, DPM from Honeygo Podiatry. Our doctor will assess your condition and provide you with quality foot and ankle treatment.
Peripheral artery disease (PAD) is when arteries are constricted due to plaque (fatty deposits) build-up. This results in less blood flow to the legs and other extremities. The main cause of PAD is atherosclerosis, in which plaque builds up in the arteries.
Symptoms
Symptoms of PAD include:
- Claudication (leg pain from walking)
- Numbness in legs
- Decrease in growth of leg hair and toenails
- Paleness of the skin
- Erectile dysfunction
- Sores and wounds on legs and feet that won’t heal
- Coldness in one leg
It is important to note that a majority of individuals never show any symptoms of PAD.
Diagnosis
While PAD occurs in the legs and arteries, Podiatrists can diagnose PAD. Podiatrists utilize a test called an ankle-brachial index (ABI). An ABI test compares blood pressure in your arm to you ankle to see if any abnormality occurs. Ultrasound and imaging devices may also be used.
Treatment
Fortunately, lifestyle changes such as maintaining a healthy diet, exercising, managing cholesterol and blood sugar levels, and quitting smoking, can all treat PAD. Medications that prevent clots from occurring can be prescribed. Finally, in some cases, surgery may be recommended.
If you have any questions, please feel free to contact our offices located in Perry Hall, and Fallston, MD . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Podiatrist Support for Runner’s Foot Pain

Foot pain in runners is a common issue often caused by plantar fasciitis, metatarsalgia, and stress fractures. Plantar fasciitis involves inflammation of the tissue along the bottom of the foot, while metatarsalgia refers to pain in the ball of the foot. Stress fractures result from repetitive impact and overuse. Stretching can help ease discomfort, including the seated towel stretch to improve flexibility and rolling a frozen water bottle under the arch to reduce inflammation. Wearing properly fitted running shoes with good support is essential. A podiatrist can evaluate pain, identify the underlying cause, recommend targeted stretches and footwear, and provide treatment to promote healing and prevent further injury for long-term foot health. If you have foot pain from running, it is suggested that you consult this type of doctor who can offer appropriate treatment solutions.
All runners should take extra precaution when trying to avoid injury. If you have any concerns about your feet, contact Edward Orman, DPM of Honeygo Podiatry. Our doctor will treat your foot and ankle needs.
How to Prevent Running Injuries
There are a lot of mistakes a runner can make prior to a workout that can induce injury. A lot of athletes tend to overstretch before running, instead of saving those workouts for a post-run routine. Deep lunges and hand-to-toe hamstring pulls should be performed after a workout instead of during a warmup. Another common mistake is jumping into an intense routine before your body is physically prepared for it. You should try to ease your way into long-distance running instead of forcing yourself to rush into it.
More Tips for Preventing Injury
- Incorporate Strength Training into Workouts - This will help improve the body’s overall athleticism
- Improve and Maintain Your Flexibility – Stretching everyday will help improve overall performance
- “Warm Up” Before Running and “Cool Down” Afterward – A warm up of 5-10 minutes helps get rid of lactic acid in the muscles and prevents delayed muscle soreness
- Cross-Training is Crucial
- Wear Proper Running Shoes
- Have a Formal Gait Analysis – Poor biomechanics can easily cause injury
If you have any questions, please feel free to contact our offices located in Perry Hall, and Fallston, MD . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Nerve Pain in the Foot and Tarsal Tunnel Syndrome
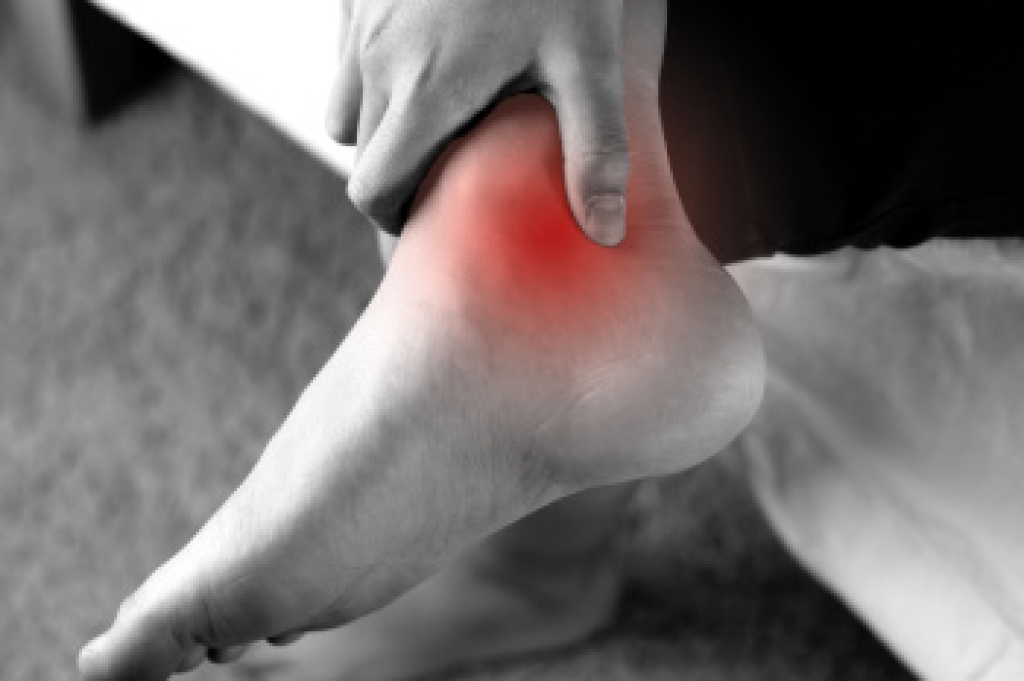
Tarsal tunnel syndrome is caused by compression of the posterior tibial nerve as it passes through the tarsal tunnel, a narrow space on the inside of the ankle. This nerve supplies sensation and movement to parts of the foot. Symptoms include burning, tingling, numbness, or shooting pain along the bottom of the foot or into the toes. Diagnosis involves a physical exam, medical history, and possibly nerve conduction studies or imaging. If you have pain in this part of your foot, it is suggested that you consult a podiatrist who can identify the condition early, and guide treatment to relieve nerve pressure and reduce symptoms, improving mobility and comfort.
Tarsal tunnel syndrome can be very uncomfortable to live with. If you are experiencing tarsal tunnel syndrome, contact Edward Orman, DPM of Honeygo Podiatry. Our doctor can provide the care you need to keep you pain-free and on your feet.
Tarsal Tunnel Syndrome
Tarsal tunnel syndrome, which can also be called tibial nerve dysfunction, is an uncommon condition of misfiring peripheral nerves in the foot. The tibial nerve is the peripheral nerve in the leg responsible for sensation and movement of the foot and calf muscles. In tarsal tunnel syndrome, the tibial nerve is damaged, causing problems with movement and feeling in the foot of the affected leg.
Common Cause of Tarsal Tunnel Syndrome
- Involves pressure or an injury, direct pressure on the tibial nerve for an extended period of time, sometimes caused by other body structures close by or near the knee.
- Diseases that damage nerves, including diabetes, may cause tarsal tunnel syndrome.
- At times, tarsal tunnel syndrome can appear without an obvious cause in some cases.
The Effects of Tarsal Tunnel Syndrome
- Different sensations, an afflicted person may experience pain, tingling, burning or other unusual sensations in the foot of the affected leg.
- The foot muscles, toes and ankle become weaker, and curling your toes or flexing your foot can become difficult.
- If condition worsens, infections and ulcers may develop on the foot that is experiencing the syndrome.
A physical exam of the leg can help identify the presence of tarsal tunnel syndrome. Medical tests, such as a nerve biopsy, are also used to diagnose the condition. Patients may receive physical therapy and prescriptive medication. In extreme cases, some may require surgery.
If you have any questions please contact our offices located in Perry Hall, and Fallston, MD . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Hammertoe Deformity and Its Common Causes

Hammertoe is a deformity where one of the smaller toes bends abnormally at the middle joint, creating a shape that resembles a hammer. This condition often results from muscle or tendon imbalances that cause the toe to remain in a bent position. Common causes include wearing tight or narrow shoes, injury, or having an unusually high foot arch. Over time, the toe may become stiff and difficult to move. Symptoms often include pain when wearing shoes, corns or calluses on the top of the toe, and redness or swelling around the joint. The deformity may start as flexible but can become rigid, if not addressed. If you have symptoms of this condition, it is suggested that you consult a podiatrist who can offer effective treatment solutions. Early recognition and treatment are important to relieve discomfort and prevent further progression that may require more advanced medical or surgical care.
Hammertoes can be a painful condition to live with. For more information, contact Edward Orman, DPM of Honeygo Podiatry. Our doctor will answer any of your foot- and ankle-related questions.
Hammertoe
Hammertoe is a foot deformity that occurs due to an imbalance in the muscles, tendons, or ligaments that normally hold the toe straight. It can be caused by the type of shoes you wear, your foot structure, trauma, and certain disease processes.
Symptoms
- Painful and/or difficult toe movement
- Swelling
- Joint stiffness
- Calluses/Corns
- Physical deformity
Risk Factors
- Age – The risk of hammertoe increases with age
- Sex – Women are more likely to have hammertoe compared to men
- Toe Length – You are more likely to develop hammertoe if your second toe is longer than your big toe
- Certain Diseases – Arthritis and diabetes may make you more likely to develop hammertoe
Treatment
If you have hammertoe, you should change into a more comfortable shoe that provides enough room for your toes. Exercises such as picking up marbles may strengthen and stretch your toe muscles. Nevertheless, it is important to seek assistance from a podiatrist in order to determine the severity of your hammertoe and see which treatment option will work best for you.
If you have any questions, please feel free to contact our offices located in Perry Hall, and Fallston, MD . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Foot Exercises to Keep Older Adults Moving

Simple foot exercises can help older adults stay steady, ease pain, and maintain mobility. As we age, feet lose strength and flexibility, which can affect balance and increase the risk of falls. Gentle movements like toe curls, ankle circles, and heel raises can improve circulation, muscle tone, and joint motion. Rolling a small ball under the foot massages sore spots and wakes up tired feet. Stretching the calves and the bottoms of the feet helps relieve stiffness. These exercises can be done seated or standing and take just a few minutes each day. They are especially helpful for those with arthritis, diabetes, or poor circulation. Staying active starts from the ground up. If you have trouble with foot pain or balance, it is suggested you see a podiatrist for treatment and additional exercise tips.
Proper foot care is something many older adults forget to consider. If you have any concerns about your feet and ankles, contact Edward Orman, DPM from Honeygo Podiatry. Our doctor can provide the care you need to keep you pain-free and on your feet.
The Elderly and Their Feet
As we age we start to notice many changes in our body, but the elder population may not notice them right away. Medical conditions may prevent the elderly to take notice of their foot health right away. Poor vision is a lead contributor to not taking action for the elderly.
Common Conditions
- Neuropathy – can reduce feeling in the feet and can hide many life-threatening medical conditions.
- Reduced flexibility – prevents the ability of proper toenail trimming, and foot cleaning. If left untreated, it may lead to further medical issues.
- Foot sores – amongst the older population can be serious before they are discovered. Some of the problematic conditions they may face are:
- Gouging toenails affecting nearby toe
- Shoes that don’t fit properly
- Pressure sores
- Loss of circulation in legs & feet
- Edema & swelling of feet and ankles
Susceptible Infections
Diabetes and poor circulation can cause general loss of sensitivity over the years, turning a simple cut into a serious issue.
If you have any questions, please feel free to contact our offices located in Perry Hall, and Fallston, MD . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Exploring the Causes of Burning Feet

Burning sensations on the bottom of the feet can arise from several underlying medical issues, including nerve damage and circulatory problems. Conditions such as peripheral neuropathy, often caused by diabetes, alcoholism, or vitamin deficiencies, also can lead to nerve hypersensitivity. This may result in persistent burning, numbness, and weakness. Poor blood flow linked to peripheral artery disease may also produce burning pain, especially during physical activity. Foot-specific conditions, including Morton’s neuroma, metatarsalgia, and tarsal tunnel syndrome can affect the nerves and soft tissues, causing intense discomfort. Infections like athlete’s foot or injuries such as fractures may provoke acute burning sensations. To determine the cause of burning foot pain a podiatrist can perform a detailed exam and order nerve conduction studies, blood tests, or imaging tests. Based on the diagnosis, treatment may involve medication, custom orthotics, or, in more advanced cases, surgery to alleviate nerve compression or restore circulation. If you experience the sensation of burning feet, it is suggested that you schedule an appointment with a podiatrist for a diagnosis and appropriate treatment.
Foot Pain
Foot pain can be extremely painful and debilitating. If you have a foot pain, consult with Edward Orman, DPM from Honeygo Podiatry. Our doctor will assess your condition and provide you with quality foot and ankle treatment.
Causes
Foot pain is a very broad condition that could be caused by one or more ailments. The most common include:
- Bunions
- Hammertoes
- Plantar Fasciitis
- Bone Spurs
- Corns
- Tarsal Tunnel Syndrome
- Ingrown Toenails
- Arthritis (such as Gout, Rheumatoid, and Osteoarthritis)
- Flat Feet
- Injury (from stress fractures, broken toe, foot, ankle, Achilles tendon ruptures, and sprains)
- And more
Diagnosis
To figure out the cause of foot pain, podiatrists utilize several different methods. This can range from simple visual inspections and sensation tests to X-rays and MRI scans. Prior medical history, family medical history, and any recent physical traumatic events will all be taken into consideration for a proper diagnosis.
Treatment
Treatment depends upon the cause of the foot pain. Whether it is resting, staying off the foot, or having surgery; podiatrists have a number of treatment options available for foot pain.
If you have any questions, please feel free to contact our offices located in Perry Hall, and Fallston, MD . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Diabetic Foot Blisters

Diabetic foot blisters, or diabetic bullae, are a rare, but important concern for people with diabetes. These fluid-filled blisters usually appear on the feet and can form without injury, often overnight. Although typically painless, they can become large and increase the risk of serious infection if not properly cared for. The exact cause is still unknown, but high blood sugar levels and diabetic neuropathy are thought to contribute. Blisters may heal on their own in a few weeks, but self-treatment can lead to complications. Infection, skin breakdown, and poor healing are real risks for diabetic patients. A podiatrist plays a key role in managing diabetic foot blisters. They can clean and protect the affected area, monitor for signs of infection, and provide foot care to prevent recurrence. Early treatment is key to avoiding more serious issues. If you have diabetic foot blisters, it is suggested that you schedule an appointment with a podiatrist for appropriate treatment.
Blisters are prone to making everyday activities extremely uncomfortable. If your feet are hurting, contact Edward Orman, DPM of Honeygo Podiatry. Our doctor can provide the care you need to keep you pain-free and on your feet.
Foot Blisters
Foot blisters develop as a result of constantly wearing tight or ill-fitting footwear. This happens due to the constant rubbing from the shoe, which can often lead to pain.
What Are Foot Blisters?
A foot blister is a small fluid-filled pocket that forms on the upper-most layer of the skin. Blisters are filled with clear fluid and can lead to blood drainage or pus if the area becomes infected.
How Do Blisters Form?
Blisters on the feet are often the result of constant friction of skin and material, usually by shoe rubbing. Walking in sandals, boots, or shoes that don’t fit properly for long periods of time can result in a blister. Having consistent foot moisture and humidity can easily lead to blister formation.
Prevention & Treatment
It is important to properly care for the affected area in order to prevent infection and ease the pain. Do not lance the blister and use a Band-Aid to provide pain relief. Also, be sure to keep your feet dry and wear proper fitting shoes. If you see blood or pus in a blister, seek assistance from a podiatrist.
If you have any questions, please feel free to contact our offices located in Perry Hall, and Fallston, MD . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Common Causes of Second Toe Pain

Second toe pain can result from several underlying conditions that place stress on the front of the foot. One frequent cause is capsulitis, which is the inflammation of the ligament capsule at the base of the second toe. This condition often leads to pain, swelling, and a sensation of instability. Bunions, which form at the base of the big toe, can also contribute by shifting pressure toward the second toe, causing discomfort and alignment changes. Another potential cause is metatarsalgia, a condition marked by inflammation and pain in the ball of the foot due to increased pressure on the metatarsal bones. If you have second toe pain, it is suggested that you consult a podiatrist who can offer relief and management tips.
Toe pain can disrupt your daily activities. If you have any concerns, contact Edward Orman, DPM of Honeygo Podiatry. Our doctor can provide the care you need to keep you pain-free and on your feet.
What Causes Toe Pain?
Most severe toe pain is caused due to a sports injury, trauma from dropping something heavy on the toe, or bumping into something rigid. Other problems can develop over time for various reasons.
Toe pain can be caused by one or more ailments. The most common include:
- Trauma
- Sports injury
- Wearing shoes that are too tight
- Arthritis
- Gout
- Corns and calluses
- Hammertoe
- Bunions
- Blisters
- Ingrown toenails
- Sprains
- Fractures (broken bones)
- Dislocations
When to See a Podiatrist
- Severe pain
- Persistent pain that lasts more than a week
- Signs of infection
- Continued swelling
- Pain that prevents walking
Diagnosis
In many cases the cause of toe pain is obvious, but in others, a podiatrist may want to use more advanced methods to determine the problem. These can range from simple visual inspections and sensation tests to X-rays and MRI scans. Prior medical history, family medical history, and any recent physical traumatic events will all be taken into consideration for a proper diagnosis.
Treatment
Treatments for toe pain and injuries vary and may include shoe inserts, padding, taping, medicines, injections, and in some cases, surgery. If you believe that you have broken a toe, please see a podiatrist as soon as possible.
If you have any questions please contact our offices located in Perry Hall, and Fallston, MD . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Blog Archives
- 2025
- 2024
- 2023
- 2022