Gout, a form of arthritis caused by the buildup of uric acid crystals in the joints, can be debilitating and painful. However, incorporating regular exercise into your routine can help manage symptoms and improve overall well-being. Low-impact activities such as walking, swimming, and cycling are gentle on the joints and can help reduce inflammation and stiffness associated with gout. It is beneficial to aim for at least 30 minutes of moderate exercise most days of the week to reap the benefits. Strength training exercises focusing on the muscles surrounding the affected joints can help improve stability and support, reducing the risk of gout attacks. Additionally, maintaining a healthy weight through regular exercise and a balanced diet can help decrease uric acid levels in the body, potentially preventing gout flare-ups. By incorporating regular exercise into your lifestyle, you can effectively manage gout and enjoy improved joint health and mobility. If you have developed gout, it is strongly suggested that you are under the care of a podiatrist who can help you manage this painful condition, which may include gentle exercise.
Gout is a foot condition that requires certain treatment and care. If you are seeking treatment, contact Edward Orman, DPM from Honeygo Podiatry. Our doctor will treat your foot and ankle needs.
What Is Gout?
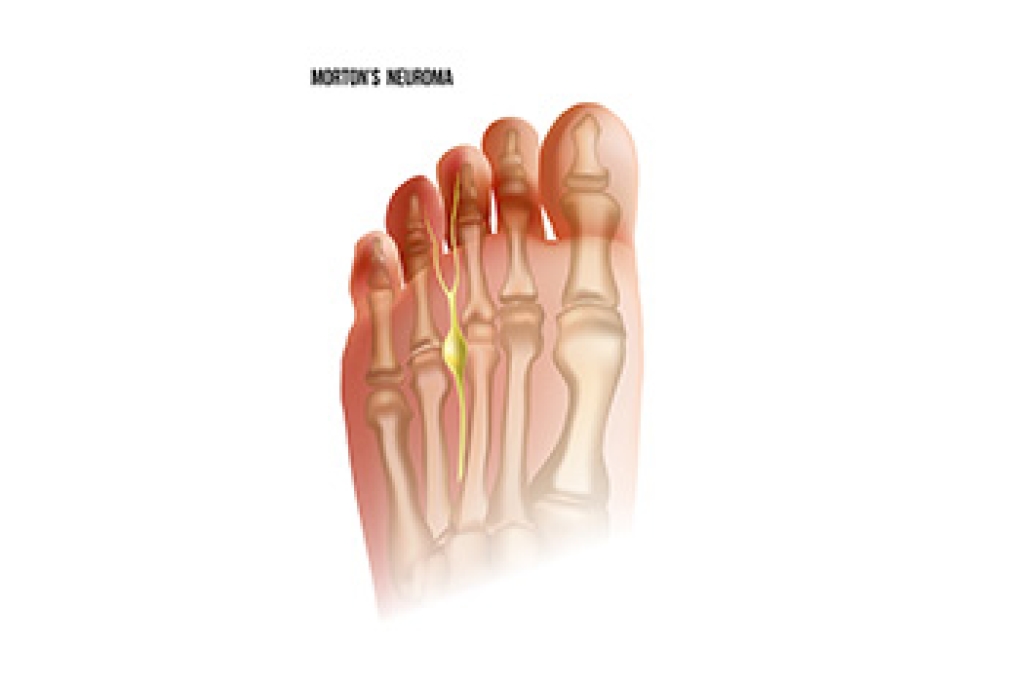
Gout is a type of arthritis caused by a buildup of uric acid in the bloodstream. It often develops in the foot, especially the big toe area, although it can manifest in other parts of the body as well. Gout can make walking and standing very painful and is especially common in diabetics and the obese.
People typically get gout because of a poor diet. Genetic predisposition is also a factor. The children of parents who have had gout frequently have a chance of developing it themselves.
Gout can easily be identified by redness and inflammation of the big toe and the surrounding areas of the foot. Other symptoms include extreme fatigue, joint pain, and running high fevers. Sometimes corticosteroid drugs can be prescribed to treat gout, but the best way to combat this disease is to get more exercise and eat a better diet.
If you have any questions, please feel free to contact our offices located in Perry Hall, and Fallston, MD . We offer the newest diagnostic and treatment technologies for all your foot care needs.