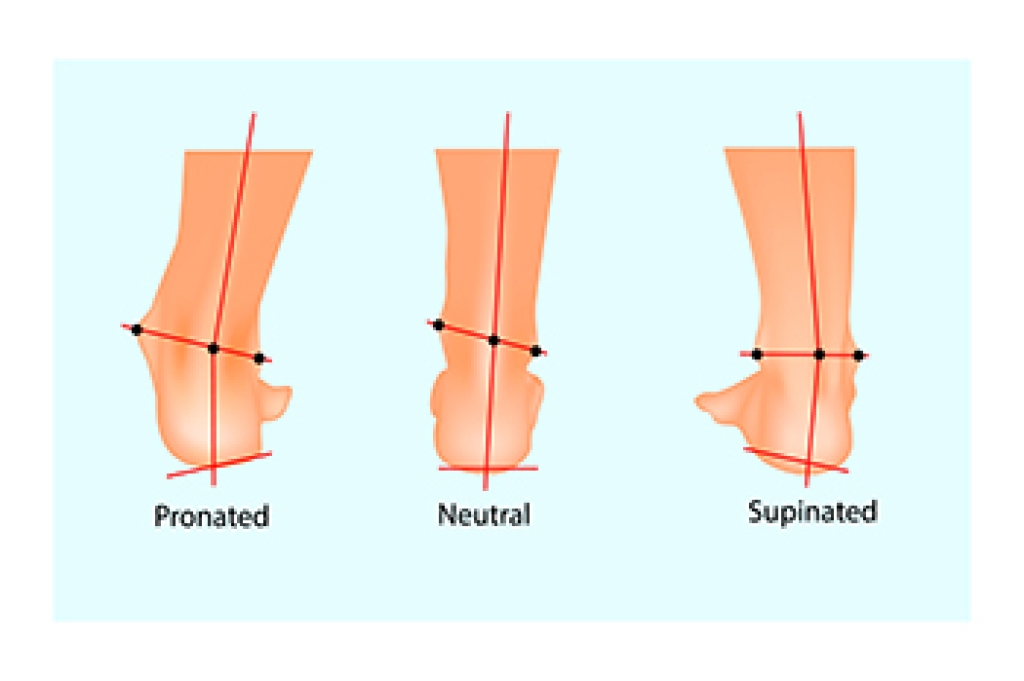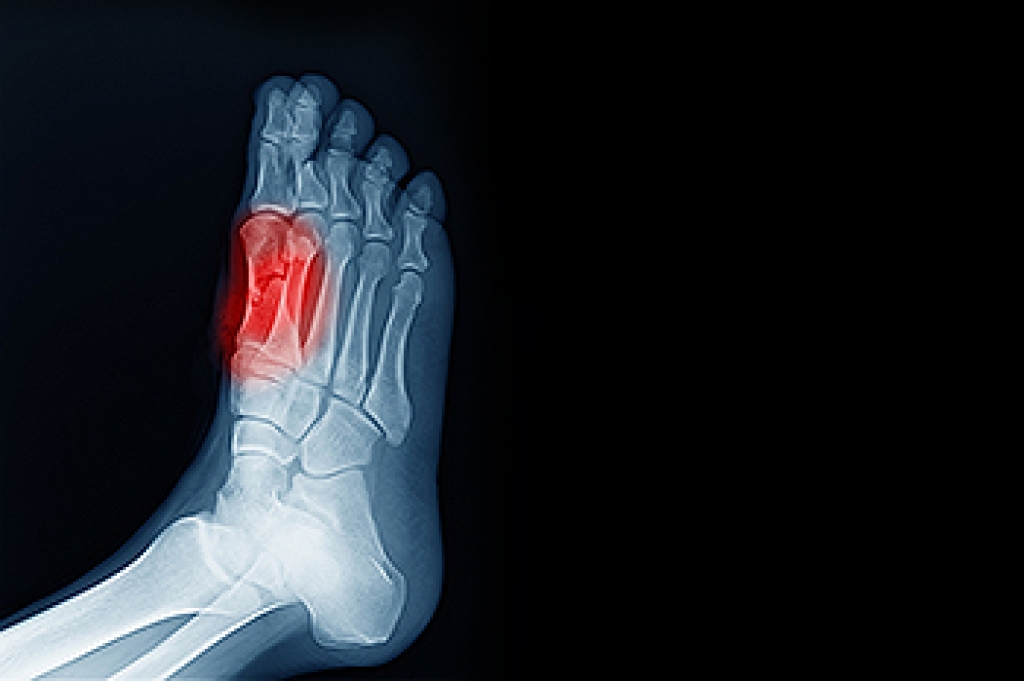
Sesamoiditis, a condition that impacts the tiny sesamoid bones beneath the big toe joint, unveils itself as inflammation in this delicate area. These small, pea-shaped bones play a vital role in weight-bearing and facilitating smooth movement of the foot. Sesamoiditis typically arises from overuse or repetitive stress on the forefoot, particularly common among athletes engaging in activities that involve frequent pushing off the toes. Ballet dancers, runners, and individuals participating in high-impact sports are often susceptible. The condition may also be triggered by structural abnormalities in foot anatomy, such as having a high arch, or from wearing improper footwear that fails to adequately cushion and support the ball of the foot. Recognizing the causes of sesamoiditis helps individuals take preventive measures, including wearing proper footwear, and modifying activities to protect these small yet significant bones in the intricate structure of the foot. Sesamoiditis is a condition that is treated by a podiatrist. If you have developed this condition, it is strongly urged that you schedule an appointment with this foot doctor who can offer you effective treatment options.
Sesamoiditis is an unpleasant foot condition characterized by pain in the balls of the feet. If you think you’re struggling with sesamoiditis, contact Edward Orman, DPM of Honeygo Podiatry. Our doctor will treat your condition thoroughly and effectively.
Sesamoiditis
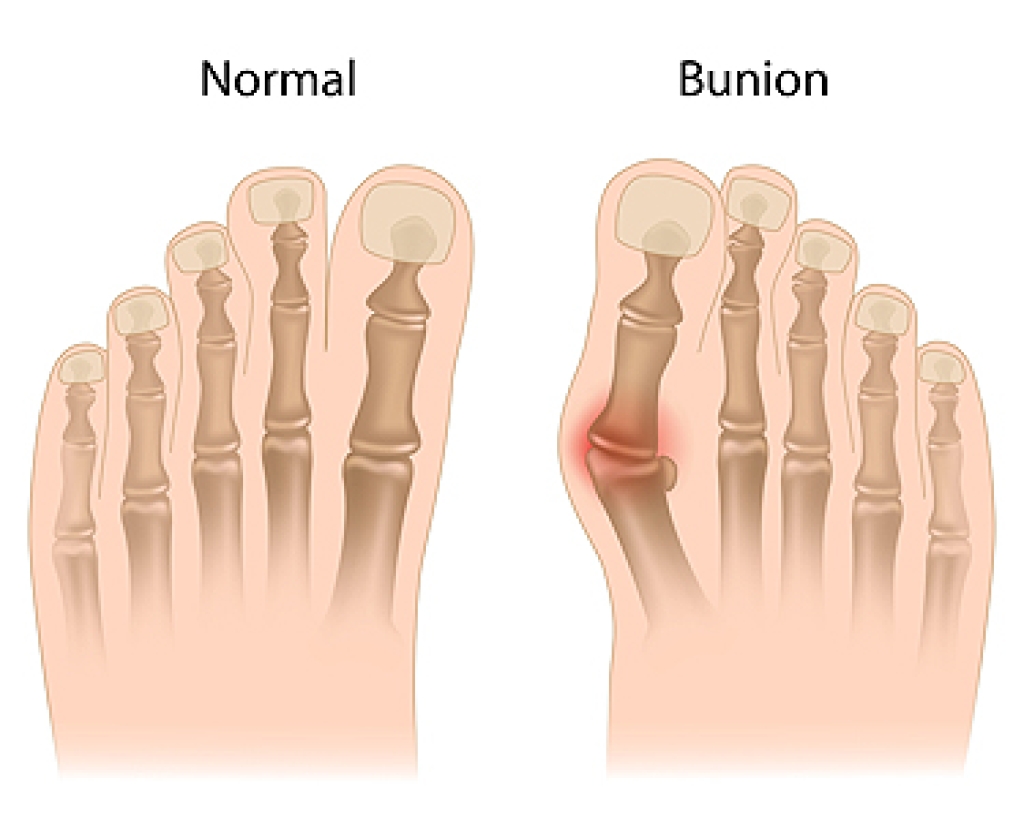
Sesamoiditis is a condition of the foot that affects the ball of the foot. It is more common in younger people than it is in older people. It can also occur with people who have begun a new exercise program, since their bodies are adjusting to the new physical regimen. Pain may also be caused by the inflammation of tendons surrounding the bones. It is important to seek treatment in its early stages because if you ignore the pain, this condition can lead to more serious problems such as severe irritation and bone fractures.
Causes of Sesamoiditis
- Sudden increase in activity
- Increase in physically strenuous movement without a proper warm up or build up
- Foot structure: those who have smaller, bonier feet or those with a high arch may be more susceptible
Treatment for sesamoiditis is non-invasive and simple. Doctors may recommend a strict rest period where the patient forgoes most physical activity. This will help give the patient time to heal their feet through limited activity. For serious cases, it is best to speak with your doctor to determine a treatment option that will help your specific needs.
If you have any questions, please feel free to contact our offices located in Perry Hall, and Fallston, MD . We offer the newest diagnostic and treatment technologies for all your foot care needs.